Do We Need an “OBGYN for Men”?
As traditional healthcare channels reveal gaps in serving the unique needs of men, a new cadre of digital health startups is stepping up to fill the void.
Discussions about gender disparities in medicine often veer towards the challenges women face—and rightly so. But the fact is, men are not spared from one enormous gender gap: life expectancy.
Men have higher mortality rates at every age. On average, male life expectancy in the U.S. at birth stands at 73.2 years, which is about six fewer years than women. This is even worse for Black (66.7 years) and Native American (61.5) men. The gender gap is not unique our country. In fact, every country — both developing and developed — with reliable health statistics report that women live longer than men.
There’s some irony in the fact that while men are the “default” in the healthcare system, hold a disproportionate number of leadership roles, and get 98.1% of venture funding, that it doesn't translate into better healthcare outcomes for them.
In this deep-dive, I wanted to untangle the complex threads of men’s health, and explore what has been done, what is being done, and most importantly, what should be done. I cover:
Why men have a lower life expectancy
Why we need an “OBGYN for men” specialty
Why urologists aren’t the answer
How startups are stepping up
Erectile dysfunction: the gateway healthcare experience?
Five massive opportunities in men’s health
Let's be absolutely clear: shining a spotlight on men's health in no way undermines or dismisses the deeply entrenched systemic issues that disproportionately affect women, particularly BIPOC women. The historical and ongoing inequities faced by women across multiple dimensions—including health—are both real and urgent. Acknowledging the gaps in men's healthcare does not diminish the critical work that needs to continue for women. But looking at women's health can also give us a sort of roadmap for what's achievable in men's health, too. It's not an either/or situation; both can—and should—get better.
Why men have lower life expectancy
What accounts for the life expectancy gap between men and women in the U.S.?
A combination of factors comes into play:
Men are more likely to die of heart disease
Men are more likely to die from risky behaviors like drinking and driving, not wearing a helmet while biking, smoking, and drug use
Men outnumber women in deadly jobs including logging, fishing, construction, and mining
Men are more likely to be victims (and perpetrators) of violent crime
Men die by suicide neary 4x more than women
Men at all ages are less likely to seek medical care and less likely to comply with medical instructions
Men are more likely to die from Covid-19
Men are less likely to have strong social networks which negatively impacts health
Some researchers hypothesize that because the Y chromosome is smaller and carries fewer genes than the X chromosome, men might have fewer genetic tools to combat disease
The shocking thing is, the leading causes of male mortality are largely preventable, underscoring the urgent need for a targeted, comprehensive approach to men's health.
Why we need an “OBGYN for men” specialty
Longevity is only part of the equation. For many men, quality of life is compromised by myriad health issues, including stress, substance use, infertility, hair loss, sexual dysfunction, obesity, and unaddressed mental health conditions. The alarming statistic that men are nearly four times more likely to die by suicide than women speaks volumes about an unspoken mental health emergency within this demographic.
Some people have also pointed to the sparse frequency of routine screenings for men, in contrast to the annual recommendations women receive (mammograms, pap smears, etc.), which further exposes them to delayed diagnoses and treatment. In fact, there are 12 preventive screenings recommended by the USPSTF for men compared to 19 for women (and an additional five during pregnancy).
These are the preventive screenings recommended by the U.S. Preventive Services Task Force (USPSTF). All these services have received an “A” or a “B” (recommended) grade from the Task Force.
Dr. Brad Gill of the Cleveland Clinic explained it to me, “Starting with pediatrics, primary care teams are charged with screening and prevention. However, once females hit reproductive age, they usually also start seeing a gynecologist, which provides them with further focus on screening and prevention for a number of conditions, including cervical cancer and breast cancer. Men don’t have a similar pathway in the healthcare system, so they rely entirely on primary care for this, especially at younger ages. That is, if they regularly see a primary care provider, which is a big IF for many men”.
Speaking of medical avoidance: a Cleveland Clinic survey found that 65% of men tend to delay seeing a doctor as long as possible when experiencing symptoms or injury. This pattern extends into mental health services, where only 37% of men with diagnosed mental illnesses opt for treatment, compared to 51% of their female counterparts.
65% of men tend to delay seeing a doctor as long as possible when experiencing symptoms or injury.
Hone Health CEO Saad Alam explained it to me: “Men hate hearing bad news. We’d rather not hear bad news and put it off than hear it and have to deal with it. Also men generally associate the doctor with bad things. It’s a cultural problem. You go to doctor when things are broken. Which is why proactive healthcare is so needed in this country”.
Telehealth seems like a perfect solution to most of these barriers… yet telehealth usage remains higher amongst women than men.
This medical procrastination, whether fueled by cultural stigmas or systemic gaps, underlines the enormous opportunity for a new care delivery approach tailored for men. Saad believes what it’s going to take is a multi-faceted approach including primary care physicians, urologists, mental health specialists, and endocrinologists, and of course somehow coordinating all this care. Saad said, “And that is very, very difficult to do”.
What about urologists?
There is no established medical specialization for men’s health, and no, urology alone cannot solve this problem. There are 13,044 urologists in the U.S., short of the 14 ,400 urologists that HHS projected to be necessary to meet the demand (in contrast, there are 35,586 OBGYNs).
Urologists primarily focus on diseases of the urinary tract (in men and women) and the male reproductive system. They do vital work but lack the more comprehensive approach seen in women's OBGYN care. Urologist Dr. Brad Gill shared, “The reality is, there is a shortage of urologists in the healthcare workforce, so in many places it is a challenge for them to just keep up with the problems patients come in with, leaving them less time to talk about screening and prevention.”
Plus, while women are recommended annual visits to their OBGYN from early adulthood, there is no such mandate for men to regularly see urologists. Add to that the fact that many urologists require a referral from your PCP, meaning preventive care is out of the question.
While women are recommended annual visits to their OBGYN from early adulthood, there is no such mandate for men to regularly see urologists. Add to that the fact that many urologists require a referral from your PCP, meaning preventive care is out of the question.
This discrepancy, coupled with the cultural stigma many men feel about discussing their health, often results in late diagnosis and treatment. There's a gap in the system that urology alone cannot fill.
How startups are stepping up
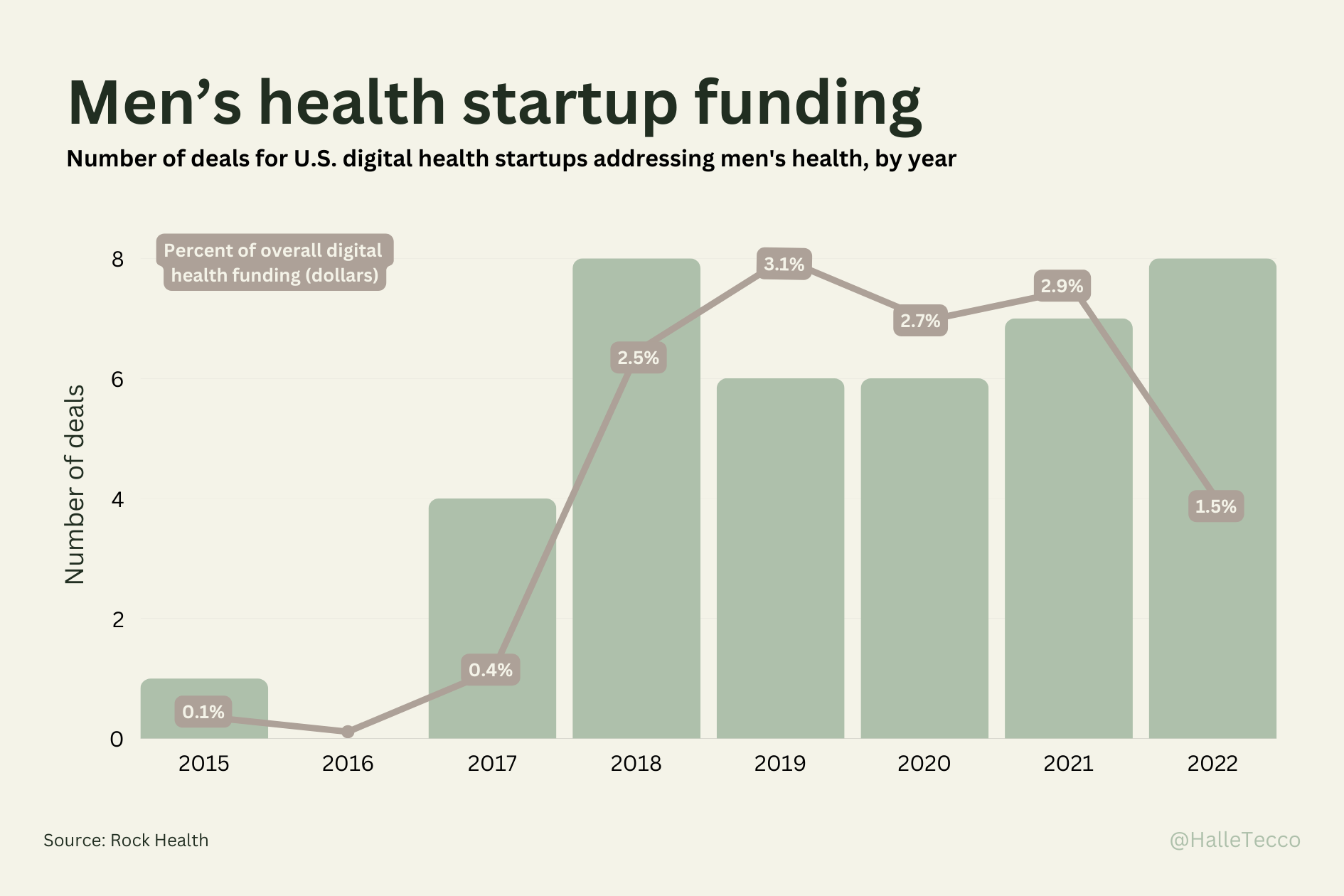
There has been some activity in the venture space over the last six years with digital health startups focused on men’s health. Men’s health companies raised $853.2M across seven deals in 2021, compared to $1.4B across 37 deals for women’s health companies.
As traditional healthcare channels reveal gaps in serving the unique needs of men, a new cadre of digital health startups is stepping up to fill the void. Through telehealth services, at-home diagnostics, and personalized care plans, these companies are increasing access to men's healthcare in a way that is both culturally resonant and more accessible (albeit mostly out of pocket).
Digital health startups focusing on men's health are working to overcome common barriers men face when seeking medical care, such as inconvenience and stigma. Telehealth for issues ranging from hair loss to erectile dysfunction to infertility help remove the discomfort many men feel in discussing such matters in person. These virtual platforms make it easier for men to proactively seek help at the early stages of health issues.
Erectile dysfunction: the gateway healthcare experience?
Erectile dysfunction (ED) could serve as a crucial entry point for men into the healthcare system. Turns out, while men hesitate to see a healthcare provider for general health reasons, they tend to be more proactive when the issue impacts their sexual performance.
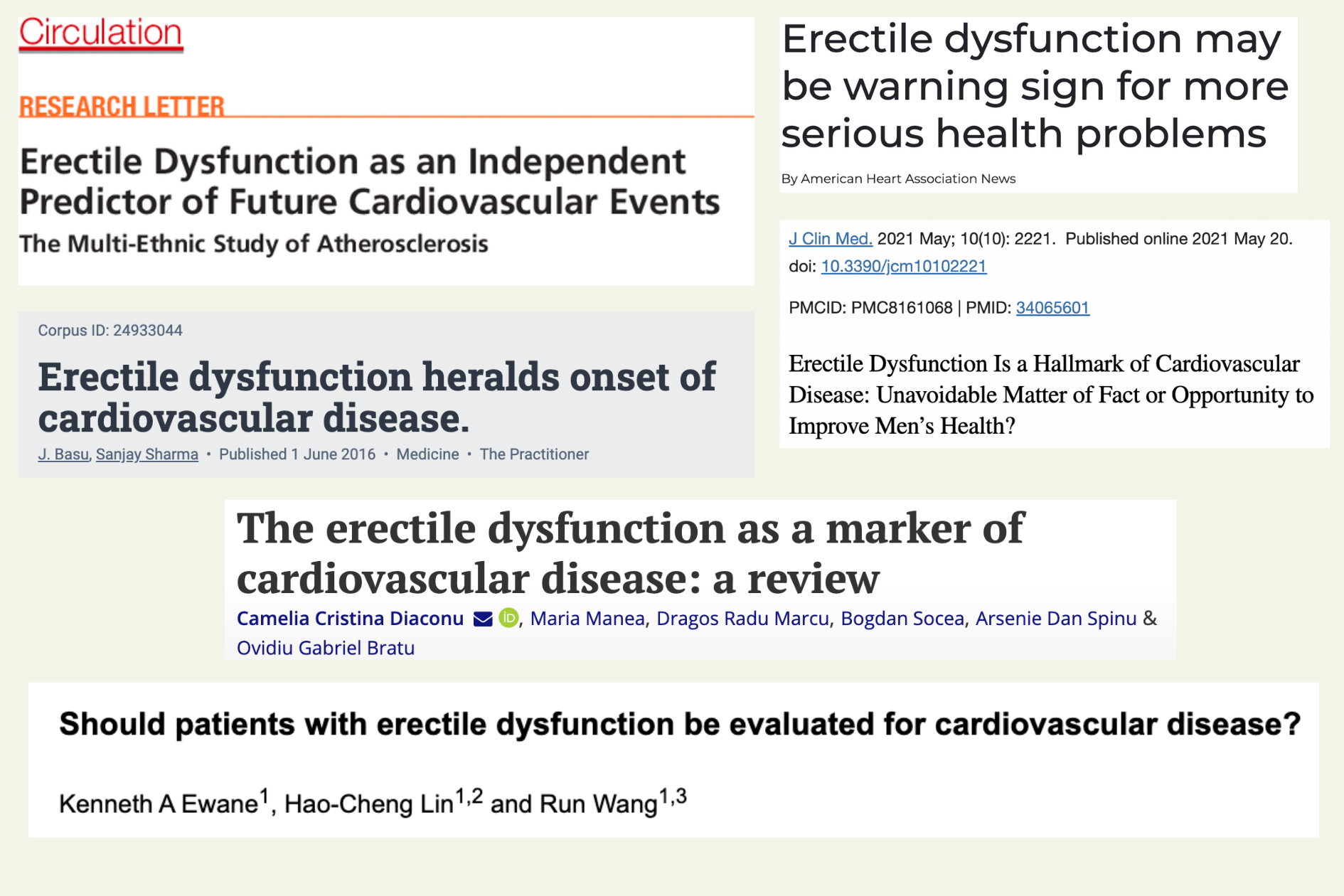
The physiology of an erection involves a finely coordinated series of vascular events, and any disruption in this flow may be indicative of broader circulatory issues. In this way, ED is a gateway to broader healthcare for men because it is actually a symptom of other health problems (diabetes, heart disease, high blood pressure, kidney disease, anxiety, depression, etc.).
According to the American Heart Association, ED could be a warning sign of current or future heart problems. It's a situation not unlike chest pain, which leads many men to seek immediate medical attention, albeit the former is often shrouded in more stigma.
The founder of Ro knows this first hand, and has spoken publicly about how his ED turned out to be a heart condition diagnosis at a young age. Companies like his have not only brought this taboo subject into the daylight but have created platforms that can potentially engage men in a broader health dialogue. When men visit these platforms for ED, they might also encounter information about related cardiovascular risks, or be prompted to monitor other key health metrics. This goes beyond the mission of merely making healthcare more accessible; it may also elevate awareness and education around interconnected health issues.
However, some healthcare folks share concerns that the ease of obtaining ED treatments could encourage men to overlook the necessity of a comprehensive health evaluation. The digitization of healthcare should not absolve individuals of the responsibility to undergo complete medical check-ups.
That’s why I was excited to see Hims recently announce Heart Health by Hims after recognizing that 30% of customers have one or more factors that can put them at higher risk for developing CVD in their lifetime. So they’re now offering a single-pill combination therapy that can address both ED and high cholesterol simultaneously. They posit that simplifying medication regimens can significantly improve adherence.
I think ED is an issue that can either draw men further into managing their whole health, or lead them down a rabbit hole of quick fixes and neglected underlying health issues. As men’s health startups continue to occupy this space, I hope to see them further integrate immediate treatment with broader healthcare engagement.
Five massive opportunities in men’s health
We’re starting to move from just prescribing pills for quick fixes to platforms that offer an integrated care model including preventive health screenings and mental health services. Here are some areas within men’s health that I’m super excited about:
1. Preventive screenings
Everyone suffers from what is called our “sick-care system”, where incentives are aligned with the treatment of diseases after they've already manifested versus preventing them in the first place. This reactionary approach not only strains our healthcare resources but also undermines the quality of life for individuals across the board.
The men’s health sector should expand to include more preventive screenings, viewing men not just as consumers in a marketplace but as patients within an ecosystem.
I spoke with tech and healthcare investor Chamath Palihapitiya about why he's bullish on the space. "Men are navigating a less-defined path in medicine with respect to routine annual screenings," he said. "As such, there's untapped potential here for preventive care that could be life-saving. That's why we've been working on a Stage 0 test for bladder cancer and will soon extend our work to other cancers."
2. Mental healthcare
An enormous opportunity in the space that few are addressing is men’s mental health. Yes, the mental health space is bursting with exciting behavioral health startups (Headspace, Brightside, Talkspace, Lyra). But it’s unclear if they’ve solved for the fact that men are less likely to seek mental health care in the first place.
According to the American Psychological Association, men are far less likely than women to seek help for disorders such as depression, substance abuse, and stressful life events due to social norms, reluctance to talk, and downplaying symptoms.
One new app for men’s mental health called Mental (which has nearly 500 five-star reviews in the App Store) acknowledges that men aren’t into existing mental healthcare options, even stating “No talk therapy required” in their marketing. The founder Anson Whitmer, PhD (who was previously head of data at Calm) told me, “It isn't just that men are hesitant to try existing solutions, it’s that they are much more likely to bounce when they do. For example, half of men drop out of therapy. And the main reason they give is that they do not resonate with the approach, usually because it is primarily feeling focused over problem-solution focused.”
I hope the next wave of innovation in men's mental healthcare can help build strategies that break down the stigma and cultural barriers deterring men from utilizing mental health services in the first place.
(It’s worth adding a side note that there are broader societal implications of increasing access to mental healthcare for men, too. One Stanford study found that men with a history of mental illness are more likely to be incarcerated after losing access to health care, concluding that better access to mental healthcare can reduce crime in a community).
3. Substance use disorder
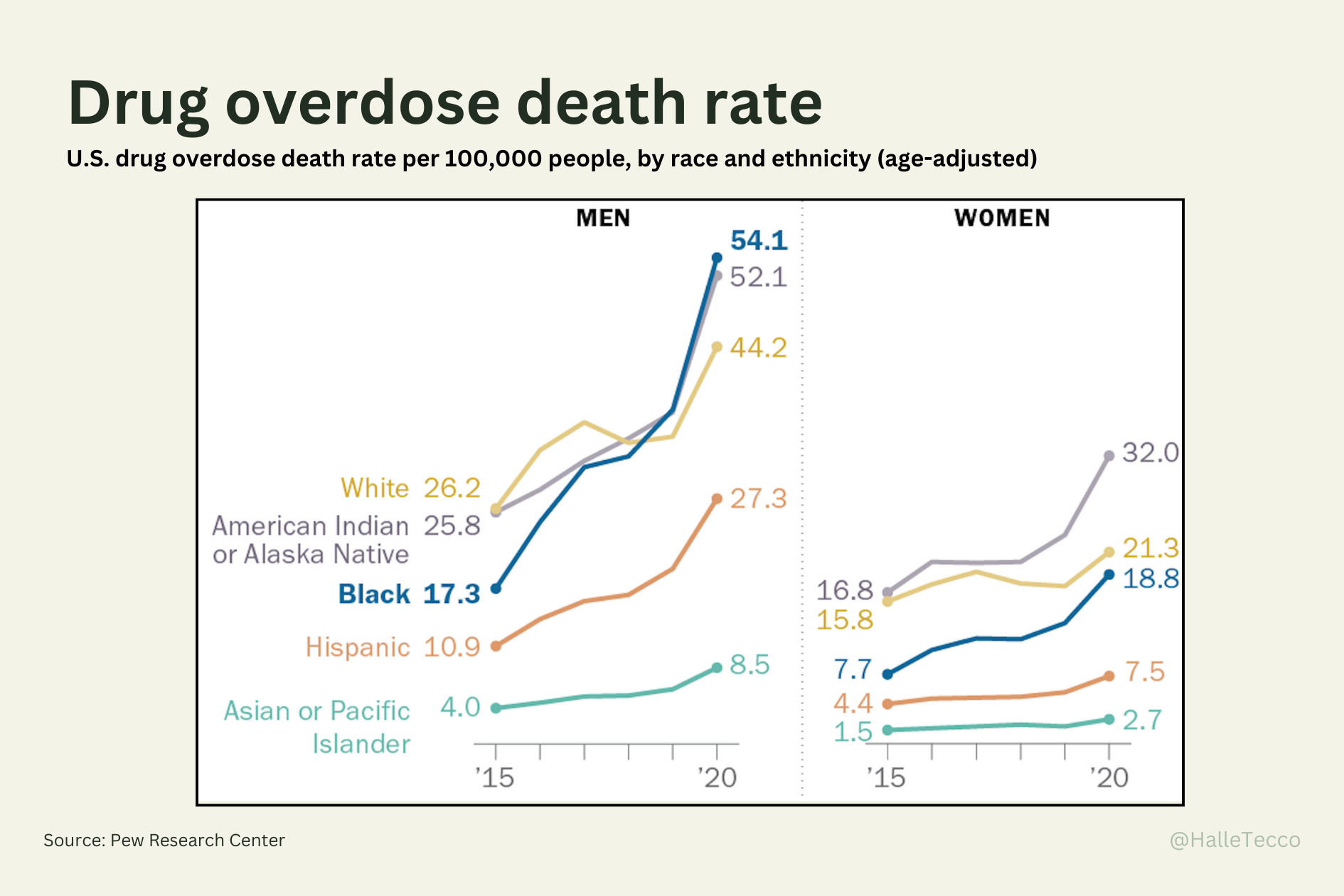
Substance use disorder is generally part of the mental health / behavioral health bucket, but deserves it’s own call-out here given the magnitude of the problem. Data suggest that men are more likely than women to engage in the use of nearly all types of illicit drugs, and the fallout is sobering: the rate of drug overdose deaths is 2-3x higher among men compared to women. 70% preventable opioid overdose death victims are male, and Black men have been hit the hardest.
This is not merely a behavioral or criminal issue; it's a public health crisis. By focusing on substance use disorder, we can do more than just treat symptoms; we can address some of the root causes that are compromising men's health at large. Tackling this problem not only has the potential to significantly extend life expectancy for men but also to improve the quality of those lives and contribute to broader societal well-being.
4. Heart health
Heart disease is the number one killer of men and women, but twice as many men die of cardiovascular diseases. According to the American Heart Association, heart disease tends to manifest about 10 years earlier in men. Yet 90% of heart disease is entirely preventable.
What Hims is doing for heart health is a great example of moving towards a more comprehensive care model that is still more accessible.
The next frontier in men's heart health must lie in prevention. What's on the horizon could well be a multifaceted approach that unifies lifestyle modification, genetic risk assessments, and data-driven, personalized health strategies.
5. Male fertility
In the last four decades, global sperm counts have plummeted by 50%, and the quality of sperm has seen a steep decline, with 1 in 20 men facing reduced fertility.
For couples struggling to get pregnant, a third of infertility cases are caused by male reproductive issues, a third by female reproductive issues, and a third caused by both partners or unknown factors. Yet fertility doctors (reproductive endocrinologist, or REIs) are trained OBGYNs first, as REI is a subspecialty in that field. Starting from this point, more of their training is focused on treating females, which may be why it seems some doctors are more inclined to treat the female first, before acknowledging the male’s role in the issue.
Men need to be more considered in the process, as they are often not educated on how to participate, and are sometimes ignored entirely outside of obtaining a sperm sample. (I talk more about this in 8 Reasons Fertility Care Is Utterly Broken).
Dr. Kevin Stephens Jr thinks it’s time we begin educating primary care physicians on male fertility. “I mostly have to refer my male patients to fertility clinics which are geared toward women and are often booked far out”. He thinks this could expand access to fertility testing in the primary care setting.
Summing it up
It's clear that men are missing proactive, comprehensive care tailored to their unique needs. The gender gap in life expectancy and mental health are but the symptomatic outgrowths of a system that has traditionally viewed men through a narrow clinical lens, often neglecting preventive care and mental well-being. In a world burgeoning with medical innovations and technological advancements, we can no longer afford this oversight.
Startups are doing the essential work of plugging the gaps, but theirs is a nascent endeavor that requires broader systemic change. This innovation must be accompanied by policy and public health initiatives that not only encourage men to actively participate in their health care journey but also equip them with the tools to do so.
And let's not forget, any substantive shift in men's health outcomes will necessitate a radical transformation in our cultural perspectives — breaking down the stigma that hinders men from seeking timely medical and psychological help.
Men's health is not just a 'men's issue'; it's a human issue, with implications that ripple across families, communities, and our society at large. Enough with the blind spots, let's get men's health in focus.